Access to healthcare in prisons is a fundamental human right, protected by the U.S. Supreme Court’s landmark decision in Estelle v. Gamble (1976). Yet, systemic issues leave many incarcerated individuals without the care they need. Here’s a quick breakdown:
- Legal Obligation: Prisons must provide adequate medical care under the Eighth Amendment.
- Current Challenges:
- Chronic illnesses often go untreated.
- Emergency care is delayed, causing preventable deaths.
- Mental health needs are neglected.
- Cultural misunderstandings lead to poor care.
- Solutions:
- Use telemedicine to reduce delays and improve access.
- Partner with local healthcare providers for specialized services.
- Leverage tools like Impact Justice AI to advocate for better conditions.
Improving prison healthcare not only protects individual rights but also strengthens public health as inmates reintegrate into society. Let’s explore the legal, ethical, and practical steps needed to address these urgent issues.
How Do Inmates Access Medical Services in a Correctional Facility?
Laws and Ethics in Prison Healthcare
Navigating the legal and ethical aspects of prison healthcare is crucial to tackling its systemic challenges. This area operates within a mix of international guidelines and domestic laws that set minimum care standards.
Global Rights Standards
The United Nations’ Mandela Rules outline key principles for prison healthcare worldwide. These rules focus on equal access to care, medical independence, respect for cultural differences, and preventive healthcare measures. Their goal is to ensure humane treatment for incarcerated individuals. While these international standards provide a baseline, U.S. laws add more specific obligations for correctional facilities.
U.S. Legal Requirements
In the U.S., prison healthcare is shaped by the Eighth Amendment, which prohibits cruel and unusual punishment. The landmark case Estelle v. Gamble established that ignoring serious medical needs constitutes such punishment. The concept of "deliberate indifference" – when authorities knowingly neglect critical medical issues – is central to this legal framework.
As stated in Estelle v. Gamble:
"An inmate must rely on prison authorities to treat medical needs; failure to do so may result in pain, suffering, or even death." [2]
Prisons are required to provide access to qualified medical professionals, address serious health concerns, maintain proper medical records, and ensure ongoing care. This obligation extends to mental health services and requires cultural awareness to address the diverse needs of incarcerated individuals effectively.
Advocacy efforts have introduced innovative tools to monitor and improve healthcare conditions in prisons. For example, Impact Justice AI is being used in Georgia’s prison system to document healthcare access issues and communicate them to decision-makers, helping push for necessary changes.
Even with these legal frameworks in place, many prisons struggle to meet the required standards, leaving gaps in care that demand urgent attention.
sbb-itb-25113a2
Main Obstacles to Prison Healthcare
Providing proper healthcare in prisons comes with serious challenges that directly affect the well-being of incarcerated individuals. These issues make it difficult to meet required medical standards and uphold basic human rights.
Space and Budget Issues
Overcrowded prisons and limited budgets mean that many inmates are left without the care they need. For instance, 20% of state prison inmates and 68% of local jail inmates with medical conditions don’t receive necessary treatment [4]. This happens because facilities often lack the space, equipment, and supplies to meet demand.
Gaps in Staff Training
The quality of prison healthcare isn’t just about resources – it’s also about the skills and training of medical staff. Many healthcare providers in prisons are not adequately trained to handle the specific needs of incarcerated populations. For example, cultural competency training, which helps staff address the diverse health needs of inmates, is often missing. This leads to miscommunication and delays in care [1].
Balancing Security and Medical Needs
Strict security protocols frequently clash with the need for timely medical treatment. Research from the ACLU shows that security concerns often take priority over healthcare, resulting in:
| Security Measures | Impact on Healthcare |
|---|---|
| Restricted Access | Emergency care is delayed or unavailable due to security rules |
| Disrupted Treatment | Ongoing care plans are interrupted by security procedures |
To address these challenges, prisons need to find ways to balance security requirements with the responsibility to provide proper medical care. This involves rethinking priorities and ensuring that healthcare is treated as a fundamental right, not a secondary concern.
New Ways to Improve Prison Healthcare
Efforts to improve healthcare in prisons are taking a new direction, focusing on technology, collaboration with local providers, and advocacy tools. These approaches aim to tackle long-standing issues while ensuring access to adequate medical care for inmates.
Remote Medical Services
Telemedicine, supported by tools like electronic health records (EHRs), is changing how inmates access healthcare. It allows consultations with specialists without requiring inmates to leave the facility, addressing both security concerns and logistical challenges. Here’s how it makes a difference:
| Service Type | Impact on Care |
|---|---|
| Virtual Consultations | Cuts down wait times for specialists by 60% |
| Remote Monitoring | Ensures continuous care for chronic conditions |
By reducing delays and improving care coordination, telemedicine is streamlining healthcare in prisons. Pairing this with partnerships with local healthcare providers can further improve the quality and accessibility of care.
Local Health Partnerships
Working with local healthcare providers broadens access to better services. For example, Roadrunner Health Services employs local professionals who understand the unique needs of their communities, ensuring more personalized care [3].
As Yang from the Harvard Gazette explains:
"Countries leading on correctional health are those that view prisoner health as part of public health more broadly." [5]
This approach has proven effective in areas like:
- Mental health services
- Treatment for substance use disorders
- Preventive care programs
- Staff training focused on cultural understanding
These partnerships not only improve care but also integrate prison healthcare into the larger public health framework.
Impact Justice AI Support
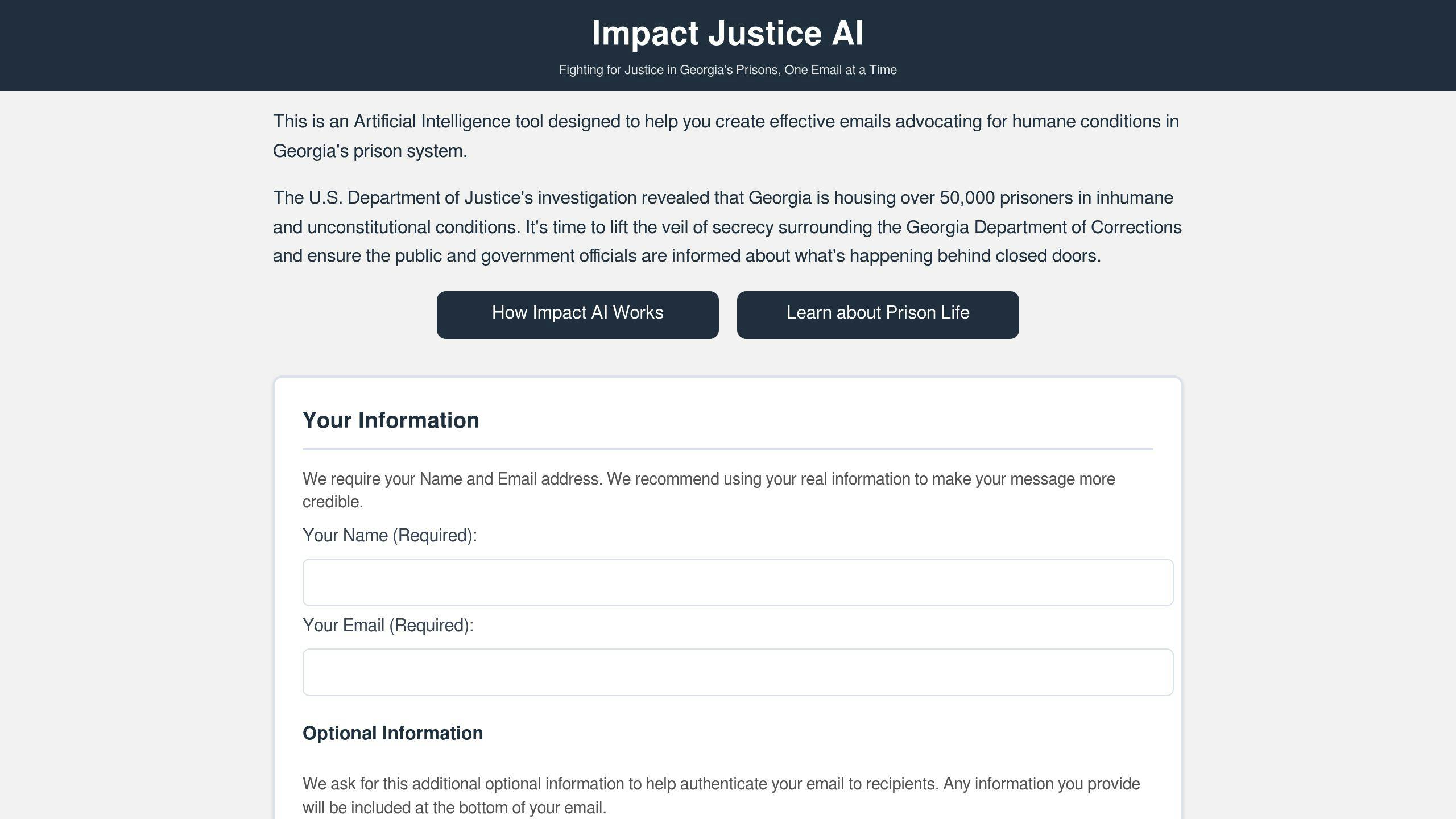
Advocacy tools like Impact Justice AI are helping push for better healthcare in prisons. This platform uses data from Department of Justice reports and investigative journalism to create evidence-based messages for decision-makers. It supports:
- Direct communication with officials and media
- Development of fact-based advocacy materials
- Monitoring and tracking advocacy efforts
Conclusion
Key Takeaways
The case of Estelle v. Gamble established the constitutional right to healthcare for incarcerated individuals, emphasizing the need to prevent unnecessary pain and suffering in prisons. Today, legal mandates, workforce considerations, and modern tools are shaping the way healthcare is provided in correctional facilities.
| Area | Progress | Challenges |
|---|---|---|
| Legal Framework | Constitutional protections exist | Gaps in implementation remain |
| Workforce Development | Local hiring models are emerging | Training remains inadequate |
| Technology | Telemedicine is on the rise | Infrastructure still lags |
Though progress is evident, major hurdles remain. Addressing these requires focused efforts to ensure all incarcerated individuals receive the care they are entitled to.
Steps for Improvement
Advancing prison healthcare calls for collaboration among healthcare professionals, advocates, and policymakers. Here are some actionable strategies:
- Leverage tools like Impact Justice AI to create advocacy materials that resonate with decision-makers.
- Provide expanded training to healthcare staff, focusing on cultural awareness and sensitivity.
- Push for broader use of telemedicine and electronic health records (EHRs) to overcome logistical barriers and improve care delivery.
Adopting approaches like Roadrunner Health Services’ local hiring model [3] can improve cultural understanding while expanding healthcare access.
Viewing prisoner health as a part of public health is essential. By combining advocacy and practical solutions, we can work towards a system that ensures constitutional rights translate into meaningful healthcare for incarcerated individuals.
